The evolution of wearable technology has been nothing short of meteoric. What began as a niche market for step-counters and fitness trackers has exploded into a mainstream phenomenon of sophisticated, multi-sensor devices that serve as constant companions on our wrists. These modern marvels are no longer just about optimizing workouts or tracking sleep; they represent a fundamental shift in personal health management. By providing a continuous stream of biometric data, wearables are moving us from a reactive model of healthcare—treating sickness as it arises—to a proactive and preventive one. Powered by advanced sensors and intelligent algorithms, these devices are becoming indispensable tools for identifying potential health issues long before symptoms become apparent. This article delves into the technology behind this revolution, its real-world impact on detecting critical conditions like atrial fibrillation, and the future of an integrated AI-driven wellness ecosystem.
The Sensor Fusion Powering Proactive Health Monitoring
The ability of a smartwatch or fitness band to provide meaningful health insights is not magic; it’s the result of a sophisticated interplay between advanced hardware and intelligent software. At the core of this capability lies a suite of miniaturized sensors working in concert to capture a detailed picture of your body’s inner workings. The latest Wearables News consistently highlights the increasing accuracy and variety of these sensors, which form the foundation of modern preventative health tech.
Photoplethysmography (PPG): The Heart of the Matter
The green lights that periodically flash on the underside of your wearable are the most visible component of its primary heart-monitoring technology: photoplethysmography, or PPG. This optical technique works by shining LED light onto the skin of your wrist. Blood is red because it reflects red light and absorbs green light. When your heart beats, the blood flow in your wrist capillaries increases, causing greater green light absorption. Between beats, the absorption lessens. The wearable’s photosensors measure the rate of these changes in light reflection, allowing it to calculate your heart rate with remarkable accuracy. However, its capability extends far beyond a simple beats-per-minute count. By analyzing the minute variations in time between each heartbeat—a metric known as heart rate variability (HRV)—the device’s AI can detect patterns of irregularity. A highly erratic and disorganized pattern is a key characteristic of atrial fibrillation (AFib), and it is this analysis that powers the irregular rhythm notifications sent by many leading devices.
Beyond the Pulse: The Role of ECG and Other Sensors
While PPG is excellent for continuous, passive background monitoring, more advanced wearables now include an electrocardiogram (ECG or EKG) sensor for on-demand, clinical-grade readings. Unlike PPG, which measures blood flow, an ECG measures the heart’s electrical signals directly. By touching a finger to the device’s crown or bezel, the user completes an electrical circuit, allowing the sensor to generate a single-lead ECG waveform. This data is far more detailed than PPG and can more definitively identify signs of AFib. This dual-sensor approach creates a powerful system: the PPG algorithm acts as a wide net, constantly scanning for potential issues, while the ECG feature serves as a more precise tool for verification. This trend is a major focus in Health & BioAI Gadgets News. Furthermore, this sensor fusion extends to other components, including accelerometers for fall detection, SpO2 sensors for blood oxygen saturation, and skin temperature sensors. Each data point adds another layer to the user’s holistic health profile, creating a rich dataset for AI analysis.
The AI Engine: Translating Raw Data into Actionable Alerts

Collecting terabytes of raw sensor data is useless without the ability to interpret it. This is where artificial intelligence and machine learning become critical. The algorithms inside these devices, often processed on the device itself thanks to advancements in AI Edge Devices News, are trained on vast, medically validated datasets. They learn to distinguish between the noisy, chaotic signals of a potential arrhythmia and benign irregularities caused by exercise or stress. The AI’s role is not to provide a diagnosis—a crucial distinction—but to function as an intelligent screening tool. It excels at pattern recognition on a scale no human could manage, identifying statistically significant deviations from a user’s baseline or known markers of disease. When a high-confidence anomaly is detected, the system generates a “nudge”—an alert prompting the user to take further action, such as performing an ECG or consulting a physician. This entire process is a prime example of the powerful applications highlighted in AI Monitoring Devices News and AI Sensors & IoT News.
Bridging the Gap: Wearables in the Clinical Pathway
The true value of a health wearable is realized when its data transcends the screen on your wrist and becomes a catalyst for clinical action. These devices are increasingly serving as a vital bridge between daily life and professional medical care, empowering users and providing physicians with unprecedented longitudinal data. They are changing the narrative from episodic care to continuous health awareness, with profound real-world consequences, particularly in cardiology.
Case Study: Detecting Silent Atrial Fibrillation
Consider a hypothetical but highly realistic scenario. A 62-year-old man, an avid cyclist who considers himself healthy, receives an irregular rhythm notification on his smartwatch overnight. He feels perfectly fine and is initially inclined to dismiss it as a fluke. However, the notification persists. Following the device’s instructions, he performs an on-demand ECG reading, which the watch flags as inconclusive but suggests sharing with a doctor. He exports the PDF of the waveform and sends it to his primary care physician through a patient portal. Intrigued by the data, the physician schedules an appointment and, upon review, orders a 12-lead clinical ECG and a 48-hour Holter monitor study. The results confirm the wearable’s suspicion: he has paroxysmal (intermittent) atrial fibrillation. This condition had been asymptomatic, meaning he would likely have been unaware of it until a more serious event, such as a stroke, occurred. Thanks to the wearable’s initial nudge, he is now on an appropriate treatment plan to manage his risk. This journey from a passive data point to a life-altering diagnosis showcases the profound impact of this technology.
Understanding the Numbers: Accuracy and Predictive Value
For these devices to be trusted by both consumers and clinicians, their alerts must be reliable. A key metric used to evaluate screening tools is Positive Predictive Value (PPV), which answers the question: “If a user receives an alert, what is the probability that they actually have the condition?” Large-scale studies have demonstrated that when a wearable’s irregular pulse notification is followed by an on-device ECG that also indicates signs of AFib, the PPV can be remarkably high—often exceeding 80% or 90%. This level of accuracy is crucial for ensuring that users and doctors take the alerts seriously. It is equally important to manage the issue of false positives, which can cause unnecessary anxiety. Manufacturers fine-tune their algorithms to strike a balance, aiming to minimize false alarms without missing true events. The core message remains consistent: the device is a highly sophisticated screening tool designed to start a conversation with a healthcare professional, not to replace one.
The Expanding Universe of Wearable Health and AI Integration
While cardiac health has been the flagship application for advanced wearables, it is merely the beginning. The same principles of continuous sensing and AI-driven analysis are being applied to a much broader spectrum of health and wellness domains. The future of personal health is an integrated ecosystem where data from various sources converges to create a truly personalized and predictive experience, a vision frequently explored in AI Research / Prototypes News.

From Sleep Tracking to Mental Wellness
The next frontier for wearables is the nuanced world of mental and emotional well-being. Devices are already leveraging metrics like HRV, resting heart rate, respiratory rate, and sleep cycle data to provide insights into stress levels and recovery. As reported in AI Sleep / Wellness Gadgets News, advanced sleep tracking can now identify the duration and quality of Deep, REM, and Light sleep stages, offering actionable advice for improving sleep hygiene. Some platforms are introducing features that actively measure electrodermal activity to quantify stress responses in real-time. This data can then trigger prompts for guided breathing exercises or mindfulness sessions, transforming the device from a passive monitor into an active wellness coach. This evolution is a key topic in discussions around AI Companion Devices News and AI for Accessibility Devices News, where technology aids in managing daily well-being.
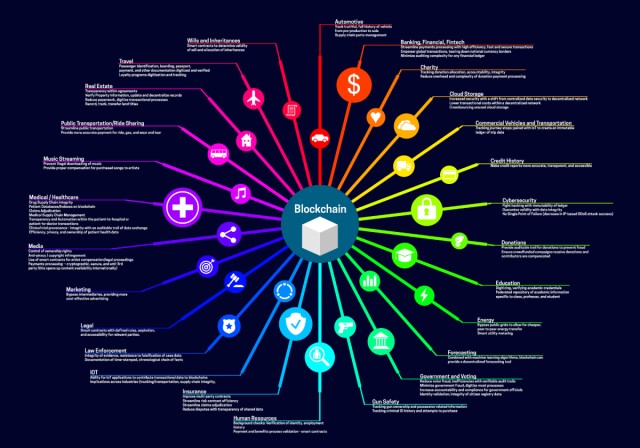
Integration with the Broader AI Ecosystem
The ultimate power of wearable data will be unlocked when it is seamlessly integrated with the wider ecosystem of smart devices. Imagine a future where your wearable communicates with your smart home. This isn’t just a topic for Smart Home AI News; it’s a tangible future. For instance, after detecting a poor night’s sleep, your AI Lighting Gadgets News-featured smart lights might adjust their color temperature in the morning to help regulate your circadian rhythm. Data on your daily activity could inform your AI Kitchen Gadgets News-connected smart refrigerator to suggest recipes that meet your caloric needs. The principles of sensor fusion and AI are universal, linking developments in Robotics News and even Autonomous Vehicles News, which rely on similar real-time data processing. The fashion world is also taking note, with AI in Fashion / Wearable Tech News exploring smart fabrics that could provide even more comprehensive biometric data than a wrist-worn device. Even emerging technologies like those seen in Smart Glasses News and Neural Interfaces News are poised to incorporate health monitoring as a core feature.
A User’s Guide to Health Wearables: Maximizing Benefits, Minimizing Anxiety

Owning a powerful health monitoring device comes with both opportunities and responsibilities. To make the most of this technology, users must approach it with the right mindset, understanding its capabilities and its limitations. Navigating this new landscape requires a blend of technological literacy and self-awareness.
Best Practices for Users
- Understand the Tool: The most critical best practice is to remember that your wearable is a screening tool, not a diagnostic one. It is designed to detect potential issues and prompt you to seek professional medical advice. Never use it to self-diagnose or to ignore symptoms.
- Context is Key: A single anomalous reading is not necessarily a cause for alarm. Factors like stress, caffeine, poor sleep, or even a software glitch can cause unusual data points. Look for persistent trends or repeated alerts before becoming concerned.
- Engage with a Professional: If you receive a health alert, the correct course of action is always to consult a doctor. Modern wearables make it easy to export and share data, such as an ECG PDF, which can be an invaluable starting point for a clinical investigation.
- Ensure Proper Fit and Use: For optical sensors like PPG to work correctly, the device must have a snug, comfortable fit on your wrist. A loose band can allow external light to interfere with the sensor, leading to inaccurate readings.
Common Pitfalls and Considerations
- Data Anxiety: For some individuals, constant access to biometric data can lead to a form of health anxiety, where they become overly focused on every minor fluctuation. It’s important to use the data as a guide, not as a source of stress.
- False Security: Conversely, a lack of alerts should not be interpreted as a clean bill of health. These devices are not foolproof and do not monitor for all conditions, such as heart attacks. If you feel unwell, seek medical attention regardless of what your device says.
- Privacy and Security: Your health data is among the most sensitive personal information you have. Before using a device, understand its privacy policy. As AI Security Gadgets News often reports, it’s crucial to know how your data is being collected, stored, and used by the manufacturer.
Conclusion: The Dawn of Proactive Personal Health
Wearable technology has fundamentally transformed the landscape of personal health. By placing sophisticated, continuous monitoring capabilities on the wrists of millions, these devices have democratized access to biometric data and empowered individuals to take a more active role in their own well-being. The paradigm of “nudge, don’t diagnose” is a powerful one, leveraging cutting-edge AI and sensor technology to act as an early warning system that prompts timely clinical intervention. While not a replacement for professional medical care, wearables are an incredibly powerful supplement to it, filling the vast data gap between doctor’s visits. As the technology continues to evolve and integrate more deeply into our digital lives, it promises a future where healthcare is more personal, more predictive, and, most importantly, more proactive than ever before.